The Psychological Impact of Withdrawal: Focuses on the Mental Health Aspects Such as Anger and Aggression During Withdrawal and its Effect on Daily Life
Abstract
This study investigated the impact of recent substance use (past 6 months) on withdrawal symptoms, daily functioning, family relationships, mental health, and anger in 178 individuals undergoing addiction treatment in Northern Cyprus. A Structural Equation Model (SEM) explored the connection between withdrawal symptoms and anger outbursts. Results revealed a positive association between recent substance use and withdrawal symptoms. Increased withdrawal symptoms were linked to significant negative effects on family relationships, mental status, and daily functioning. Withdrawal symptoms were positively correlated with anger outbursts, suggesting a pathway where withdrawal triggers anger and destructive behaviours. Furthermore, a weaker but positive link was found between anger-related destructive behaviours and self-harm tendencies.
Keywords: Substance abuse, withdrawal, anger outbursts, mental health, Northern Cyprus
Introduction
In terms of American Psychiatric Association (APA) (2013) identified substance usage disorder (SUD) as a global public health problem, its several adverse impact on personal well-being, family cohesion and society. The intricate interplay of biological, psychological, and social factors makes the endeavour of addiction treatment and recovery a daunting one the presence of withdrawal symptoms constitutes a significant element of this challenge, posing a risk to treatment adherence and heightening the likelihood of relapse (Koob & Volkow, 2016).
Literature Review
Developing effective interventions for people seeking help with SUDs requires an extensive knowledge of the ways in which symptoms of withdrawal affect all facets of life. Beyond the immediate physical and psychological discomfort, withdrawal symptoms can also have far-reaching consequences for daily life functioning. Substance usage related to negative effects on social interactions, mental health, and overall well-being of life, in terms of research study (Angarita et al., 2016; Brorson et al., 2013). Furthermore, strained family relationships, a common challenge associated with SUDs, can be exacerbated during the withdrawal process, potentially hindering a key source of support during recovery (Substance Abuse and Mental Health Services Administration [SAMHSA], 2020).
The existence of signs of withdrawal during the initial phases of addictions rehabilitation is a strong indicator of an individual's mental health. Studies show links between withdrawal and increased levels of depression, anxiety, and psychological distress (Budney et al., 2004; Sofuoglu et al., 2005). In addition, withdrawal-related distress can trigger maladaptive coping mechanisms and increase vulnerability to relapse (Sinha & Li, 2007).
A growing area of inquiry focuses on the relationship between withdrawal and anger. Anger is a natural human emotion, but in the context of addiction, it can become dysregulated and manifest in outbursts (Hawkins & Blaine, 2016). Research suggests that substance withdrawal may heighten irritability and impulsive aggression (Allsop et al., 2011; Budney et al., 2003). This is concerning, as uncontrolled anger can lead to destructive behaviours, damage interpersonal relationships, and hinder the treatment process (Serafini et al., 2016).
While previous studies shed light on the detrimental effects of substance withdrawal in various domains, a more comprehensive understanding of these interrelationships is needed. Such knowledge is crucial for informing tailored treatment approaches that address withdrawal symptoms and their cascading effects, ultimately improving chances of long-term recovery.
When the above literature is examined, this study aims to examine how withdrawal symptoms affect participation in daily life, family relationships, mental status and anger and outbursts through voluntary data shared by individuals participating in a substance abuse diagnosis, treatment and follow-up program in Northern Cyprus.
Methodology
Research Aim and Questions
The study aims to contribute to a better understanding of the complex interaction between these situations in solving the health, social and economic problems related to substance use disorder. The following research questions were analysed within the scope of the research.
- RQ 1: Is there a significant relationship among the increase in the amount of preferred substance use and deprivation status, family relations, working and educational life, physical condition, mental state and participation in life?
- RQ 2: What is the relationship between withdrawal symptoms, frequency of preferred substance usage and anger levels?
- RQ 3: In terms of the SEM model, the extent to which violence and harm due to rapid anger and anger outbursts are how much affected by the level of preferred substance withdrawal?
Research Design and Data Collection Tools
In this study, The Addiction Profile Index (API) developed by Ögel et al. (2012) was used to measure multiple dimensions of substance dependency. API is a self-report questionnaire consisting of 37 items and with 5 subscales: characteristics of substance use; dependency diagnosis; the effects of substance use on the user; craving; motivation to quit using substances. This instrument is highly reliable with α=0.89 (Cronbach alpha).
Research Sample and Data Collection Procedure
Data collected from a total of 178 volunteers from an addiction diagnostic treatment program in Northern Cyprus (Detailed demographic data and descriptive statistics of the study sample are presented in the Chapter 4).
Analysis of Data
Correlational quantitative research is done to analyse the data. All analyses were performed using SPSS24 and Amos, an unpaired t-test or Pearson's χ2 test (P-value < 0.05) and structural equation modelling were used to analyse the data.
Ethical Consideration
The study has been approved by the ethics committee of the Northern Cyprus Prime Minister’s Anti-Drug Commission with regard to the Helsinki Declaration on human subjects testing. All the subjects were previously informed about the nature of the study and the data collected for the study were anonymized and processed to safeguard the privacy of participants and prevent the inclusion of any personal information.
Findings
The use of the preferred substance and withdrawal status demonstrated a positive and significant moderate correlation, wherein withdrawal symptoms gradually intensified with increased substance use in the last 6 months (p<0.05). Concurrently, the deterioration of family relationships was observed, albeit at a weak level, with a significant inverse relationship as withdrawal symptoms of the preferred substance escalated (p<0.05). The negative impact on an individual's working and educational life, with a weak moderate inverse relationship, was also evident as withdrawal symptoms increased. Furthermore, the physical condition of the individual was adversely affected by the increase in withdrawal symptoms (p<0.05). Similarly, the mental status of individuals was negatively affected at a moderate level in the opposite direction as withdrawal symptoms increased in the substances they preferred (p<0.05). Lastly, the increase in withdrawal symptoms had a negative effect on life participation (p<0.05). As the individuals experience an escalation in withdrawal symptoms associated with their preferred substances, their mental well-being is adversely impacted in a moderate manner (p<0.05). The augmentation in withdrawal symptoms has a negative effect on their engagement in life activities (p<0.05) (see table 5.1).
The heightened utilization of preferred substances over the past half year has a detrimental influence on familial relationships, educational pursuits, occupational endeavours, and physical well-being, albeit to a limited extent (p<0.05). Furthermore, the escalation in substance use over the past six months detrimentally affects their mental state and their involvement in daily life, displaying a moderate inverse correlation (p<0.05) (see table 5.2.).
Anger significantly, but slightly (p<0.05), increased positively as people's deprivation levels developed. Weak moderate uncontrollable outbursts of rage and the impulse to break objects significantly increased positively (p<0.05) as the symptoms of deprivation grew. A mild to moderate rise in rapid anger is positively significant (p<0.05) in the recent six months when the preference substance has been used more frequently. However, uncontrollably angry outbursts and the impulse to damage things significant increased at a positive moderate level (p<0.05) as the preference item was used more frequently in the last six months. It is observed that there is a positive correlation between the urge to shatter items during angry outbursts and the fast anger of substance addicts above the medium level. This correlation is high significant (p<0.05). Considering all of the aforementioned data, it can be concluded that consuming preferred goods more frequently throughout the past six months causes deprivation symptoms, which in turn causes people to become angrier more quickly. Uncontrolled outbursts of fury cause people to smash and spill things around them because they become angry faster.
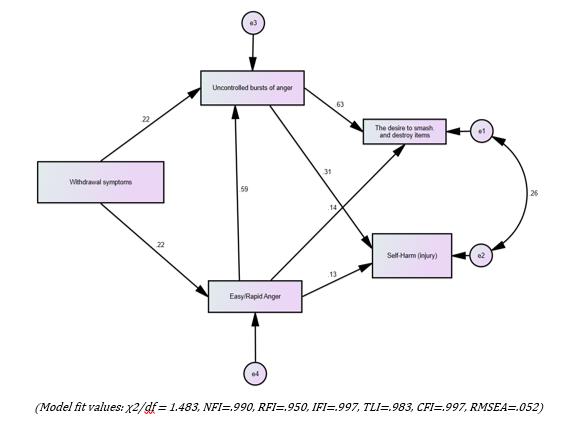
Upon examination of the model fit values, it can be observed that RMSEA has good fit values, whereas χ2/df, NFI, RFI, IFI, TLI, and CFI values have exceptional fit values. It is evident from this that the model statistically satisfies the model fit requirements (see figure 5.1.). The model's results are shown in table 5.3. below.
The augmentation in the escalation of withdrawal symptoms among individuals who partake in the diagnosis-treatment and follow-up program for substance abuse in Northern Cyprus significantly elicits rapid anger, albeit to a limited extent (p<0.05). Similarly, the amplification in withdrawal symptoms provokes episodes of anger, albeit to a limited extent (p<0.5). Uncontrollable outbursts of anger surpassing the moderate threshold are significantly triggered as a result of swift irritation (p<0.05). Consequently, the urge to shatter objects experiences a substantial increase (p<0.05). The augmentation in uncontrollable outbursts of anger significantly prompts acts of self-harm, albeit to a limited extent slightly below the moderate threshold. However, the dominance of the desire to break things over self-harm is primarily due to uncontrollable anger outbursts. In the case of deprivation, self-harm is not triggered solely by rapid anger (p>0.05). The occurrence of self-harm becomes a possibility when an uncontrollable outburst of anger arises from rapid anger. Nevertheless, the inclination to break things because of quick anger is remarkably feeble (p<0.05). Additionally, there exists a significant albeit weak correlation between the increase in the desire to break things and self-harm.
Discussion
Our findings support existing literature, highlighting the detrimental effects of withdrawal symptoms on daily life functioning, family relationships, mental status, and anger outbursts. Additionally, this study contributes by providing evidence of a potential link between withdrawal symptoms and self-harm tendencies, albeit weaker than the observed link to anger-related destructive behaviours.
The positive association between recent substance use and withdrawal symptoms aligns with established knowledge (Koob & Volkow, 2016; NIDA, 2021). As individuals abruptly cease or significantly reduce their substance intake, the body attempts to re-establish homeostasis, leading to a cascade of physiological and psychological reactions. These withdrawal symptoms can be debilitating, significantly impacting daily life activities such as work, social interactions, and self-care (Angarita et al., 2016; Brorson et al., 2013).
The discovery that the presence of withdrawal symptoms has a detrimental impact on familial relationships is in accordance with previous research that suggests substance use disorders can strain family dynamics due to the associated emotional distress, financial burdens, and behavioural disruptions (Di Sarno et al., 2021; Morita et al., 2011; Shukla et al., 2022). Additionally, the occurrence of withdrawal symptoms during the initial stages of recovery can further exacerbate these challenges, hindering effective communication and presenting additional barriers for both the individual and their family.
In addition, this study provides further support for the established connection between withdrawal symptoms and mental health issues. The observed negative correlation between withdrawal symptoms and mental well-being is in line with previous studies that have shown an increased susceptibility to depression, anxiety, and psychological distress during withdrawal (McHugh & Weiss, 2019). This finding emphasizes the significance of incorporating mental health support into addiction treatment programs to address the concurrent mental health challenges often experienced by individuals with substance use disorders.
One of the most significant contributions of this study is the exploration of the relationship between withdrawal symptoms and anger outbursts. Our findings revealed a positive association, suggesting that increased withdrawal symptomatology triggers anger and associated destructive behaviours, including the urge to break and destroy objects. This aligns with emerging research highlighting the link between withdrawal and dysregulated anger, which can manifest as irritability, aggression, and impulsive behaviours (Bonnet et.al., 2017; Gorelick et.al., 2012; Herrmann et.al., 2015). This finding emphasizes the need to address anger management within addiction treatment programs, equipping individuals with skills to manage their anger effectively and prevent destructive behaviours during withdrawal and beyond.
While the study identified a positive association between withdrawal symptoms and self-harm tendencies, the effect size was weaker compared to the link with anger-related destructive behaviours.
Conclusion
Although this study relies on a limited sample size and self-report data that are prone to error, it provides illuminating insights into the complex effects of withdrawal symptoms on the process of recovery from addiction. In addition to physical symptoms, withdrawal has detrimental effects on areas such as daily functioning, family relationships, mental health and anger management. Therefore, in addition to addressing withdrawal symptoms, addiction treatment strategies should also target overall well-being during the treatment process. Furthermore, more work is needed to understand the link between withdrawal symptoms and self-harm tendencies. Addiction rehabilitation programs that address these complex issues can better prepare people for long-term recovery and well-being.
Challenges and Limitations of the Study
This study has several limitations. First, many of the outcomes were self-report variables. This method has inherent limitations, and objective measurements may be required to evaluate aspects of withdrawal that are hard to evaluate from self-reported surveys. Second, the sample size is small therefore the findings may have limited generality. Third, almost all subjects were men, and the findings may not entirely generalize to women.
It is important to use larger, more diverse sample sizes for future studies, and objective measurements to get more accurate estimates of the percentage of substance users who are likely to have a withdrawal syndrome.
References
Allsop, D. J., Norberg, M. M., Copeland, J., Fu, S., & Budney, A. J. (2011). The Cannabis Withdrawal Scale development: patterns and predictors of cannabis withdrawal and distress. Drug and alcohol dependence, 119(1-2), 123–129. DOI: 10.1016/j.drugalcdep.2011.06.003
American Psychiatric Association (APA). (2013). Diagnostic and statistical manual of mental disorders: DSM-5™ (5th ed.). American Psychiatric Publishing, Inc. DOI:
Angarita, G.A., Emadi, N., Hodges, S., & Morgan, P. T. (2016). Sleep abnormalities associated with alcohol, cannabis, cocaine, and opiate use: a comprehensive review. Addiction Science & Clinical Practice, 11, 9. DOI:
Bonnet, U., & Preuss, U. W. (2017). The cannabis withdrawal syndrome: current insights. Substance abuse and rehabilitation, 8, 9–37. DOI:
Brorson, H. H., Ajo Arnevik, E., Rand-Hendriksen, K., & Duckert, F. (2013). Drop-out from addiction treatment: A systematic review of risk factors. Clinical Psychology Review, 33(8), 1010-1024. DOI:
Budney, A. J., Hughes, J. R., Moore, B. A., & Vandrey, R. (2004). Review of the validity and significance of cannabis withdrawal syndrome. The American journal of psychiatry, 161(11), 1967–1977. DOI:
Budney, A. J., Moore, B. A., Vandrey, R. G., & Hughes, J. R. (2003). The time course and significance of cannabis withdrawal. Journal of abnormal psychology, 112(3), 393–402. DOI:
Di Sarno, M., De Candia, V., Rancati, F., Madeddu, F., Calati, R., & Di Pierro, R. (2021). Mental and physical health in family members of substance users: A scoping review. Drug and alcohol dependence, 219, 108439. DOI: 10.1016/j.drugalcdep.2020.108439
Gorelick, D. A., Levin, K. H., Copersino, M. L., Heishman, S. J., Liu, F., Boggs, D. L., & Kelly, D. L. (2012). Diagnostic criteria for cannabis withdrawal syndrome. Drug and alcohol dependence, 123(1-3), 141-147. DOI:
Herrmann, E. S., Weerts, E. M., & Vandrey, R. (2015). Sex differences in cannabis withdrawal symptoms among treatment-seeking cannabis users. Experimental and clinical psychopharmacology, 23(6), 415–421. DOI:
Koob, G. F., & Volkow, N. D. (2016). Neurobiology of addiction: A neurocircuitry analysis. The Lancet Psychiatry, 3(8), 760-773. DOI:
McHugh, R. K., & Weiss, R. D. (2019). Alcohol Use Disorder and Depressive Disorders. Alcohol research: Current Reviews, 40(1). DOI:
Morita, N., Naruse, N., Yoshioka, S., Nishikawa, K., Okazaki, N., & Tsujimoto, T. (2011). Mental health and emotional relationships of family members whose relatives have drug problems. Nihon Arukoru Yakubutsu Igakkai zasshi/Japanese journal of alcohol studies & drug dependence, 46(6), 525–541. https://pubmed.ncbi.nlm.nih.gov/22413561/
National Institute on Drug Abuse (NIDA). (2021, March 4). Drugs, brains, and behavior: The science of addiction. https://nida.nih.gov/research-topics/addiction-science/drugs-brain-behavior-science-of-addiction
Ögel, K., Evren, C., Karadağ, F., & Gürol, D. T. (2012). The development, validity, and reliability of the Addiction Profile Index (API). Turk psikiyatri dergisi/Turkish journal of psychiatry, 23(4), 263–275. https://www.turkpsikiyatri.com/PDF/C23S4/en/6.pdf
Serafini, K., Toohey, M. J., Kiluk, B. D., & Carroll, K. M. (2016). Anger and its Association with Substance Use Treatment Outcomes in a Sample of Adolescents. Journal of child & adolescent substance abuse, 25(5), 391–398. DOI: 10.1080/1067828X.2015.1049394
Shukla, A., Saurabh, Kukreti, P., & Kataria, D. (2022). Assessing financial status, legal status, employment status and social relationships in patients with complicated and uncomplicated alcohol withdrawal. Indian Journal of Psychiatry 64(3), S658. DOI:
Sinha, R., & Li, C. S. (2007). Imaging stress- and cue-induced drug and alcohol craving: association with relapse and clinical implications. Drug and alcohol review, 26(1), 25–31. DOI:
Sofuoglu, M., Dudish-Poulsen, S., Poling, J., Mooney, M., & Hatsukami, D. K. (2005). The effect of individual cocaine withdrawal symptoms on outcomes in cocaine users. Addictive behaviors, 30(6), 1125–1134. DOI:
Substance Abuse and Mental Health Services Administration (SAMHSA). (2020). Substance Use Disorder Treatment and Family Therapy: Updated 2020. Treatment Improvement Protocol (TIP) Series, No. 39. Available from: https://www.ncbi.nlm.nih.gov/books/NBK571080/
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
30 August 2024
Article Doi
eBook ISBN
978-625-98059-2-4
Publisher
Emanate Publishing House Ltd.
Volume
-
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-197
Subjects
Addiction, Substance Abuse, Northern Cyprus
Cite this article as:
Minas, M. Y. (2024). The Psychological Impact of Withdrawal: Focuses on the Mental Health Aspects Such as Anger and Aggression During Withdrawal and its Effect on Daily Life. In N. Dağlıoğlu, & S. Kılıç Akıncı (Eds.), The Landscape of Substance Abuse in Northern Cyprus: Trends, Risks, and Responses, vol -. (pp. 95-107). Emanate Publishing House Ltd.. https://doi.org/10.70020/BI.20240801.5

